Extracorporeal Shockwave Treatment
History of Extracorporeal Shockwave Therapy
Extracorporeal Shockwave Therapy (ESWT), otherwise referred to as shockwave therapy, was first introduced into clinical practice in 1982 for the management of urologic conditions. The success of this technology for the treatment of urinary stones quickly made it a first-line, non-invasive, and effective method. Subsequently, ESWT was studied in orthopaedics, where it was identified that it could loosen the cement in total hip arthroplasty revisions. Further animal studies conducted in the 1980s revealed that ESWT could augment the bone-cement interface, enhance osteogenic response, and improve fracture healing. While shockwave therapy has been shown to be beneficial in fracture healing, most orthopaedic research has focused on upper and lower extremity tendinopathies, fasciopathies, and soft tissue conditions.
Physiology
Shockwaves are sound waves with distinct physical properties, including nonlinearity, high peak pressure followed by low tensile amplitude, a rapid rise time, and a brief duration of approximately 10 milliseconds. They consist of a single pulse, a broad frequency range (0–20 MHz), and a high-pressure amplitude (0–120 MPa).
These unique characteristics create both positive and negative phases of the shockwave. The positive phase generates direct mechanical forces on the target tissue, while the negative phase induces cavitation, forming gas bubbles that implode at high velocity. This implosion produces a secondary wave of shockwaves, enhancing the mechanical impact and therapeutic potential of the treatment.
Shockwave therapy is widely used in various medical fields, particularly in musculoskeletal disorders, due to its ability to promote tissue repair and pain relief through these dynamic mechanisms.
In comparison to ultrasound waves, the shockwave peak pressure is approximately 1000 times greater than the peak pressure of an ultrasound wave.
Mechanism of Action
The exact effects of ESWT treatment are not fully understood. However, the proposed mechanisms of action include:
Promotion of neovascularisation at the tendon-bone junction
Stimulation of tenocyte proliferation
Osteoprogenitor differentiation
Increased leukocyte infiltration
Amplified growth factor and protein synthesis to stimulate collagen production and tissue remodelling
Principles of ESWT
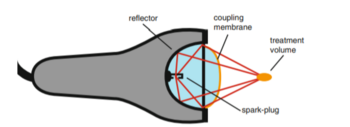
There are three different methods of generating shockwaves: electrohydraulic, electromagnetic, and piezoelectric. Despite their different mechanisms, all three methods use water as a medium to transmit shockwaves, ensuring effective energy transfer to the targeted tissues.
Shockwave therapy is widely recognised for its ability to promote tissue regeneration and reduce pain, making it a valuable tool in the treatment of musculoskeletal conditions.
Direct shockwave and indirect cavitation effects cause haematoma formation and focal cell death, which then stimulate new bone or tissue formation.
Clinical Indications
Shockwave therapy is primarily used in the treatment of common musculoskeletal conditions, including:
Upper and lower extremity tendinopathies
Greater trochanteric pain syndrome
Medial tibial stress syndrome
Patellar tendinopathy
Plantar fasciopathy
Adhesive capsulitis
Non-union of long bone fractures
Avascular necrosis of the femoral head
Osteoarthritis of the knee